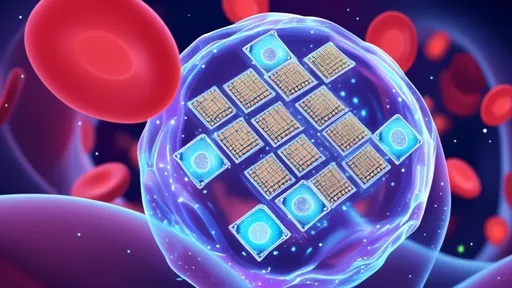
The realm of medical technology is undergoing a quiet revolution, one that might soon make traditional health monitoring devices seem as archaic as leeches and mercury thermometers. At the heart of this transformation lies an innovation so deceptively simple that it borders on science fiction: edible microchips. These tiny, ingestible sensors promise to redefine how we track our internal health metrics, offering real-time data without the need for invasive procedures or bulky wearables.
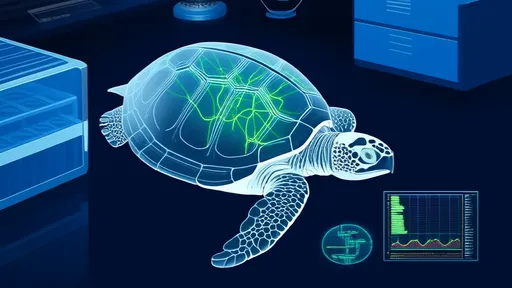
Imagine swallowing a pill that doesn’t contain medication but instead houses a microscopic laboratory capable of analyzing your digestive system, blood chemistry, or even detecting early signs of disease. This isn’t speculative futurism—it’s already happening. Researchers and startups are racing to develop edible chips that can monitor everything from gut microbiota imbalances to hydration levels, transmitting findings directly to your smartphone. The implications for preventive healthcare are staggering, particularly for chronic conditions like diabetes or hypertension where continuous monitoring is critical.
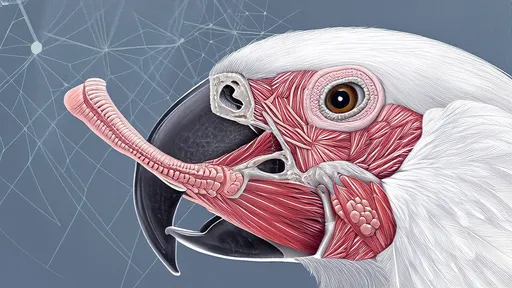
What makes these devices truly groundbreaking is their biocompatibility. Unlike traditional implants, which often trigger immune responses or require surgical insertion, edible chips leverage materials that either dissolve harmlessly or pass through the digestive tract. Some prototypes use cellulose-based circuits powered by stomach acid, while others incorporate nutrients like magnesium and vitamin B12 as conductive elements. This marriage of biology and electronics opens doors to applications beyond healthcare, including precision nutrition and pharmaceutical compliance tracking.
The data security challenges, however, are as complex as the technology itself. Transmitting sensitive health metrics wirelessly raises legitimate concerns about hacking and privacy breaches. Developers are countering these risks with advanced encryption protocols and blockchain-based verification systems. Yet, as with any connected health device, establishing consumer trust will be paramount—no one wants their digestive patterns becoming the next data breach headline.
Perhaps the most profound impact will be seen in remote and underserved regions. In areas where medical infrastructure is sparse, edible sensors could provide lifesaving diagnostics without requiring specialist visits. Field trials in rural India have already demonstrated their potential for detecting parasitic infections earlier than conventional stool tests. When paired with AI-driven analysis, these chips might eventually identify emerging health threats before symptoms manifest.
Critics rightly question whether this technology will widen healthcare disparities rather than bridge them. The current cost of production puts these devices out of reach for many, though proponents argue that economies of scale could eventually make them as affordable as a daily vitamin. Regulatory hurdles also loom large—no governing body has yet established comprehensive guidelines for ingestible electronics, leaving manufacturers to navigate uncharted ethical and safety waters.
The culinary world hasn’t ignored this trend either. Forward-thinking food scientists are experimenting with flavor-masked sensor particles that could turn functional foods into diagnostic tools. Picture your morning yogurt containing microscopic analyzers that screen for vitamin deficiencies, or your post-workout smoothie confirming muscle recovery status. This blurring line between nutrition and diagnostics heralds a future where every meal contributes to our health data ecosystem.
As research accelerates, the limitations of current prototypes become clearer. Battery life remains a constraint, with most passive designs lasting mere hours in the harsh environment of the human gut. Signal interference from dense muscle tissue complicates data transmission, and the variability of human physiology demands remarkably adaptable designs. Still, the progress made in just the past five years suggests these are engineering challenges rather than fundamental roadblocks.
The psychological dimension shouldn’t be underestimated either. Swallowing a microchip—even one made of food-grade materials—triggers visceral reactions in many people. Cultural perceptions of surveillance and bodily autonomy will shape adoption rates as much as the technology’s efficacy. Manufacturers are wisely focusing initial applications on critical care scenarios where benefits clearly outweigh philosophical concerns.
Looking ahead, the convergence of edible electronics with other emerging technologies paints an intriguing picture. Combine them with CRISPR-based biosensors and you might have chips that not only detect pathogens but trigger immune responses. Pair them with quantum dot markers and they could map tumors with unprecedented precision. The true potential lies not in standalone devices but in their integration with the broader biotech revolution.
Medical practitioners caution against viewing these as magic bullets. No sensor can replace comprehensive healthcare, and overreliance on self-monitoring tools risks creating a generation of anxious patients interpreting raw data without clinical context. The ideal scenario sees edible chips as one component in a holistic care framework—enhancing, not replacing, professional medical judgment.
Investment patterns reveal where the industry expects breakthroughs. Venture capital is flooding into startups focusing on non-invasive cancer detection via edible markers, while military contracts drive development of chips that monitor soldiers’ stress hormones in combat zones. The consumer wellness market, always hungry for the next biohacking trend, has spawned luxury versions tracking microbiome diversity for the bio-optimization crowd.
Environmental considerations add another layer of complexity. While most current designs are biodegradable, mass adoption would require stringent controls to prevent ecological contamination. The precedent of microplastics has made researchers rightly cautious about introducing any persistent synthetic materials into human waste streams. Sustainable solutions might involve chips that not only dissolve safely but actually provide nutritional value during their brief operational window.
The ethical debate extends to data ownership. Should pharmaceutical companies have access to the terabytes of physiological data these chips will generate? Can insurers demand ingestion histories as part of underwriting? Legal scholars anticipate fierce battles over what constitutes informed consent when technology operates inside a person’s body yet generates data controlled by external entities.
Technical hurdles aside, the most significant barrier may be cultural. In societies where food carries deep symbolic meaning, the idea of "eating computers" triggers unease. Religious authorities haven’t yet weighed in on whether sensor-laden substances violate dietary laws. Marketing these innovations will require careful framing—emphasizing their role as temporary diagnostic visitors rather than permanent bodily alterations.
Pioneering gastroenterologists report that patient responses during trials range from enthusiastic embrace to profound discomfort. The "yuck factor" diminishes with education, suggesting public awareness campaigns will be crucial. Interestingly, younger generations raised on fitness trackers and DNA testing show markedly less resistance, hinting at inevitable generational acceptance.
The military and space exploration sectors have emerged as unexpected testing grounds. NASA funds research into chips that monitor astronaut health during Mars missions, where traditional medical support is impossible. Special forces units trial versions that detect blood loss or shock before the operator recognizes symptoms. These extreme-environment applications often drive innovations that later benefit civilian medicine.
As with any disruptive technology, unintended consequences will emerge. Will employers start requiring "diagnostic lunches" as part of workplace wellness programs? Could divorce cases subpoena gut microbiome data as evidence of stress? The societal ripple effects extend far beyond the laboratory, challenging our definitions of privacy and bodily integrity in the digital age.
The road ahead is equal parts promising and perilous. Edible chips won’t replace blood tests or MRIs, but they could create an entirely new category of preventive medicine—one where our bodies constantly communicate their needs in a language of data. How we choose to listen, interpret, and act on that information will determine whether this becomes another passing tech fad or the foundation of genuinely personalized healthcare.
By /Jul 15, 2025
By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025
By /Jul 15, 2025
By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025
By /Jul 15, 2025

By /Jul 15, 2025

By /Jul 15, 2025