In an era where digital experiences often prioritize adrenaline and competition, a quiet revolution is emerging in the realm of serious games. End-of-life care, traditionally associated with clinical settings and somber atmospheres, has found an unlikely ally in video game design. Developers and healthcare professionals are collaborating to create healing experiences for terminally ill patients, challenging our perceptions of both gaming and palliative care.
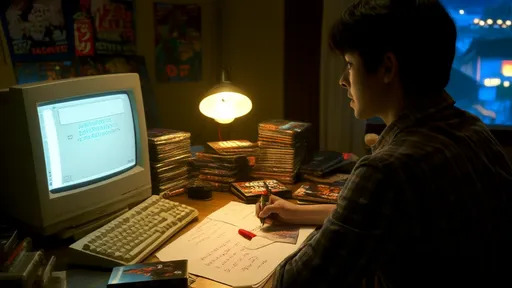
The concept might seem paradoxical at first glance – how could interactive entertainment possibly address the profound needs of those facing mortality? Yet beneath the surface lies a carefully crafted therapeutic approach. These games don't distract from life's final chapter so much as they help patients engage with it meaningfully. Through gentle gameplay mechanics and thoughtful narratives, they provide tools for emotional expression, legacy creation, and even pain management.
One remarkable example comes from a small studio that worked closely with hospice nurses. Their creation allows players to virtually revisit significant locations from their lives, not through photorealistic graphics but via abstract, impressionistic representations. A childhood home might appear as shifting blocks of color that respond to the player's breathing patterns detected through biofeedback sensors. The effect is less about accuracy and more about emotional resonance, helping patients process memories without overwhelming them.
Pain specialists have observed unexpected benefits from these interventions. The immersive quality of games appears to alter pain perception through focused attention and the release of endogenous opioids. Unlike traditional medication, this approach comes without pharmaceutical side effects. One hospital reported that patients using specially designed VR experiences required 23% less breakthrough pain medication during sessions, a finding that's prompting further research into digital analgesia.
The visual language of these games deliberately avoids medical imagery. Instead, developers employ metaphorical landscapes – a boat journey down a river might represent the passage of time, while tending a virtual garden could symbolize nurturing relationships. This symbolic approach allows patients to explore difficult emotions at one remove, making the experience feel less clinical and more personally meaningful. Therapists note that patients often initiate conversations about their condition after gameplay that they'd previously avoided during standard counseling.
Family dynamics receive particular attention in these designs. Multiplayer modes aren't about competition but creating shared memories. One poignant example allows a patient and loved ones to collaboratively build a digital constellation, with each star representing a significant moment in their shared history. The resulting artwork can be saved and revisited, becoming a therapeutic tool for anticipatory grief work. Developers report that these features often facilitate communication between family members when direct conversation feels too difficult.
Technical innovations continue to push boundaries. Eye-tracking technology enables patients with limited mobility to navigate game worlds through gaze alone. Adaptive algorithms adjust difficulty in real-time based on the player's vital signs and facial expressions. Perhaps most remarkably, some experimental systems use brain-computer interfaces to translate neural activity into in-game actions, offering agency to patients who've lost physical control. These advancements aren't just about accessibility – they're about preserving dignity and self-expression in the face of physical decline.
Ethical considerations remain paramount throughout development. Designers work closely with bioethicists to ensure these experiences never feel exploitative or promise false hope. The games avoid prescriptive narratives about "the right way" to face mortality, instead creating open-ended spaces for personal exploration. This careful balance has won over initially skeptical clinicians, many of whom now see game-based interventions as valuable complements to traditional palliative care approaches.
As research continues, early results suggest measurable impacts on quality-of-life metrics. Patients report decreased anxiety and increased feelings of peace after regular gameplay sessions. Perhaps more importantly, family members describe renewed opportunities for connection during difficult times. In one touching case, a daughter reported that playing a simple puzzle game with her dying mother gave them their first genuine laughter together in months – a moment of normalcy amidst the medical routines.
The emergence of these therapeutic games signals a broader shift in how we conceptualize both entertainment and healthcare. By blending cutting-edge technology with deep psychological insight, developers are creating spaces where patients can explore life's final journey on their own terms. In doing so, they're challenging the gaming industry to reconsider its potential – not just as a purveyor of escapism, but as a facilitator of profound human experiences at life's most vulnerable moments.
Looking ahead, the field shows promise for expansion beyond terminal cases. Researchers are exploring adaptations for chronic pain management, grief counseling, and even preventative mental health care. As the technology becomes more sophisticated and acceptance grows within medical communities, these healing virtual experiences may well become standard components of compassionate care. Their greatest achievement might ultimately be this: demonstrating that even in medicine's most emotionally complex terrain, play can have a serious purpose.

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025